
Prolapse – or Pelvic organ prolapse (POP) – is when one or more of your pelvic organs, such as your bladder, womb (uterus), or bowel—shift from their usual position and press into the walls of the vagina. It can sound alarming when you first get diagnosed with one, but the good news is that prolapse is common (as many as 1 in 2 woman have one!), treatable, and certainly nothing to be ashamed of! Many women experience prolapse symptoms at some point in their lives, and with the right support, there are plenty of ways to improve symptoms and get back to living your best life.
Why Does Prolapse Happen?
Your pelvic floor is a group of muscles and tissues that act like a supportive hammock for your pelvic organs. It helps keep them in place when more pressure is placed on them, such as when you sneeze, cough, jump, run or squat (for more about how the pelvic floor works, check out my blog here). However, if your pelvic floor is struggling or is regularly overloaded with pressure, it may struggle to hold your organs in place as it should. This can happen for a number of reasons, including:
- Pregnancy and childbirth – The pelvic floor is on double time when carrying and delivering a baby as it not only supports your growing baby, but the rest of your body as it moves differently, which can lead your pelvic floor to fatigue.
- Menopause and aging – Hormonal changes can affect the pelvic floor muscle tone and tissue strength.
- Chronic straining – Things like constipation, heavy lifting, or persistent coughing can putting extra pressure on the pelvic floor, which can lead it to fatigue over time.
- Being overweight – Extra weight increases pressure on the pelvic floor, making it work harder.
The key thing to remember? You didn’t do anything wrong! Prolapse is common, and there’s plenty you can do to feel better.
What Does Prolapse Feel Like?
Every woman’s experience of prolapse is different, and interestingly, the size of a prolapse doesn’t always match the symptoms. Some women with a mild prolapse may feel significant discomfort, while others with a larger prolapse may hardly notice it at all.
That said, some of the most common symptoms include:
- A feeling of heaviness or pressure in the vagina or lower stomach.
- A sensation like something is “falling down” or a small bulge in the vagina.
- Unable to hold onto a tampon or keep a menstrual cup in place.
- Discomfort or a dragging feeling, especially after standing for long periods.
- Changes in bladder or bowel habits, such as needing to wee more often, struggling to empty fully, or slight leaks.
- Less sensation or discomfort during sex.
These symptoms can range from barely noticeable to more bothersome, but the good news is that having symptoms doesn’t always mean the prolapse is severe—and there are plenty of effective ways to manage and improve them.
Can Prolapse Cause Back Pain?
Yes, for some women, prolapse can contribute to lower back pain. This happens because the pelvic floor and lower back muscles work together to support your body. If your pelvic floor isn’t as strong as it should be, other muscles can become overworked, leading to aches and tension. Strengthening your core and pelvic floor muscles can often help reduce or even stop back pain.
Which Type of Prolapse Do I Have?
Prolapse comes in different forms, depending on which organ is involved—and each type can cause slightly different symptoms.
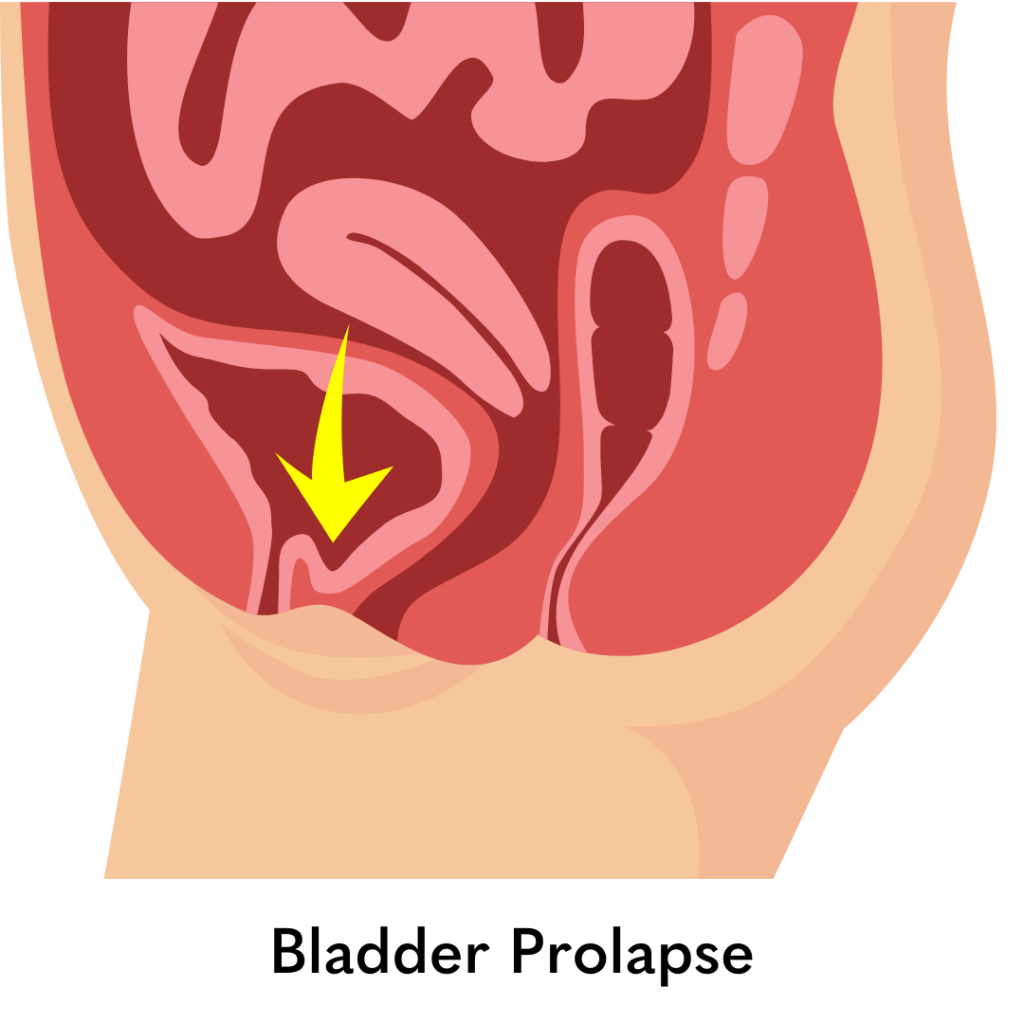
- Bladder prolapse (cystocele) – When the bladder bulges into the front wall of the vagina, it can cause a heavy feeling, difficulty emptying the bladder, or frequent trips to the loo.
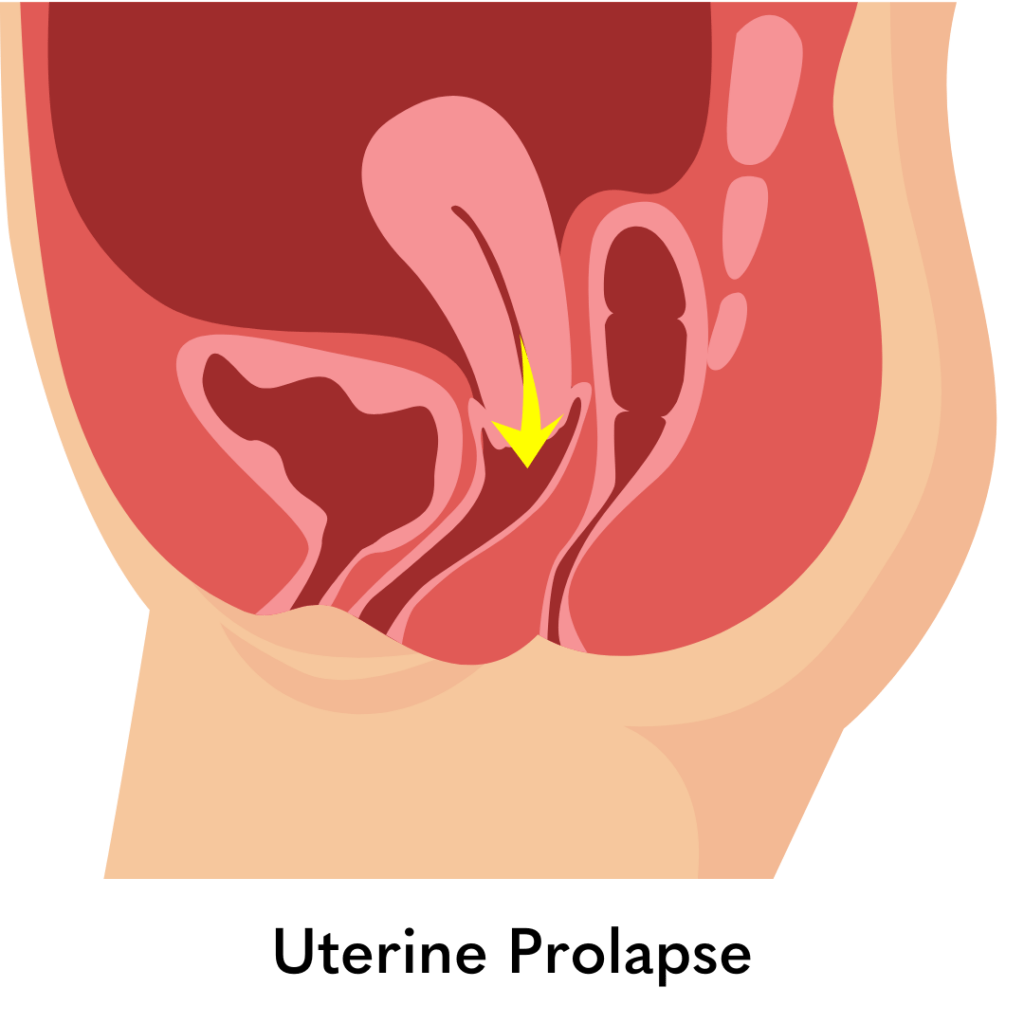
- Uterine prolapse – When the womb moves down into the vagina, it may create a dragging sensation, lower back discomfort, or a feeling of something “falling down.”
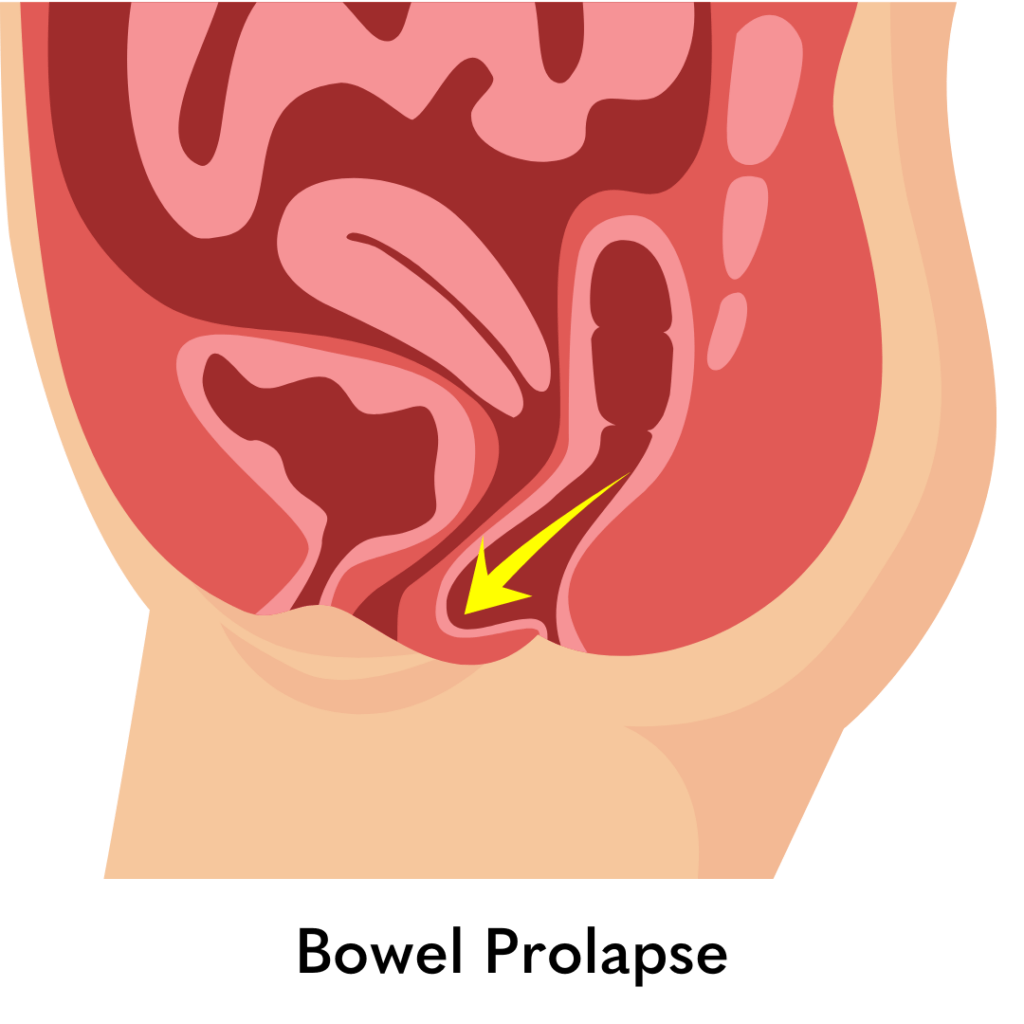
- Bowel prolapse (rectocele) – When the rectum pushes into the back wall of the vagina, it can make bowel movements feel difficult or incomplete.
- Vaginal vault prolapse – This happens when the top of the vagina sags, often after a hysterectomy, and can lead to a sensation of pressure or discomfort.
It’s important to know that prolapse isn’t always straightforward—you can have more than one type at the same time, and symptoms don’t always match the type or size of prolapse you have. Some women with a small prolapse may feel quite uncomfortable, while others with a more noticeable one might not have many symptoms at all. That’s why a proper assessment is key. The best way to manage prolapse is to understand how it’s affecting you personally and find the right approach to help you feel strong, comfortable, and in control of your body.
Will Prolapse Go Away on Its Own?
Mild prolapse can sometimes improve with lifestyle changes and strengthening exercises. However, more significant prolapse usually won’t fully disappear without some kind of intervention. The good news? There are plenty of options—from simple at-home strategies to professional support—to help you feel better and stay in control of your symptoms.
How Is Prolapse Treated?
The best approach depends on how much your prolapse is affecting you, but options include:
- Lifestyle changes – Managing constipation, exercising and maintaining a healthy weight can all make a difference.
- Pelvic floor exercises – Strengthening these muscles can help provide better support. To learn how to do a great squeeze (or kegel), go to my blog here.
- Physiotherapy – By understanding why your pelvic floor is struggling and providing tailored therapy to help strengthen your pelvic floor to feel more supported, reduce symptoms.
- Vaginal pessaries – These are small, silicone devices, which are placed inside the vagina to provide extra support for your pelvic organ and take some of the pressure off your pelvic floor. Pessaries need to be fitted by a healthcare professional, please see your GP to be referred.
- Hormone therapy – Vaginal estrogen can help improve tissue strength, especially after menopause. For more information on hormone therapy, please see your GP.
- Surgery – If, after trying all of the above, or if your symptoms are more severe, surgery may be an option to repair and support the prolapsed area.
Most women find that a combination of these approaches works well to manage symptoms and help them feel back in control.
Who Should I See for Help?
If you think you might have a prolapse, the best first step is to see your GP. They can check your symptoms, offer reassurance, and refer you to a specialist if needed. But you don’t have to wait for a referral to start getting help? A women’s health physiotherapist can be a fantastic first step in understanding what’s going on and learning how to manage your symptoms effectively.
Physiotherapy focuses on strengthening and supporting your pelvic floor, but it’s not just about squeezing those muscles! A specialist physio will assess how your whole body works together—including posture, breathing, and movement patterns—to help reduce pressure on your pelvic floor.
With the right exercises, techniques, and lifestyle adjustments, many women find their symptoms improve significantly—sometimes even avoiding the need for more invasive treatments. Whether your prolapse is mild or more advanced, working with a physiotherapist can help you feel stronger, more in control, and able to get back to doing the things you love with confidence.
The Bottom Line
Prolapse is common, and while it can be a little unsettling at first, it is treatable. You are not alone, and there are plenty of ways to manage symptoms and feel like yourself again. The most important thing? Don’t suffer in silence. Help is out there, and with the right support, you can move, laugh, and live your life without worry again.
Love what you’re reading? Sign up for Thrive’s newsletter here and get empowering pelvic health tips, inspiring success stories, and updates on our mission to make the world a leak-free zone! Don’t miss out—join the Thrive community today!